Diphtheria is an infectious disease spread by direct physical contact or breathing the aerosolizedsecretions of infected individuals. Historically quite common, diphtheria has largely been eradicated in industrialized nations through widespread vaccination[citation needed]. In the United States, for example, there were 53 reported cases of diphtheria between 1980 and 2000,[6] but only a total of 2 cases of diphtheria have been reported in the 21st century, the last of which was in 2003.[7] The diphtheria–pertussis–tetanus (DPT) vaccine is recommended for all school-age children in the U.S., and boosters of the vaccine are recommended for adults, since the benefits of the vaccine decrease with age without constant re-exposure; they are particularly recommended for those traveling to areas where the disease has not been eradicated.Hyderabadi cuisine is highly influenced by Mughlai and to some extent by French,[187] Arabic, Turkish, Iranian and nativeTelugu and Marathwada cuisines.[154][185] Other popular native dishes include nihari, chakna,baghara baingan and the desserts qubani ka meetha, double ka meetha and kaddu ki kheer (a sweet porridge made with sweet gourd).[154][188]Hyderabad's role in the pearl trade has given it the name, "City of Pearls" and up until the 18th century, the city was also the only global trading centre for large diamonds.[15][128][129]Industrialisation began under the Nizams in the late 19th century, helped by railway expansion that connected the city with major ports.[130][131] From the 1950s to the 1970s, Indian enterprises, such as Bharat Heavy Electricals Limited (BHEL), Nuclear Fuel Complex (NFC), National Mineral Development Corporation (NMDC), Bharat Electronics (BE), Electronics Corporation of India Limited (ECIL), Defence Research and Development Organisation (DRDO), Hindustan Aeronautics Limited (HAL), Centre for Cellular & Molecular Biology (CCMB), Centre for DNA Fingerprinting and Diagnostics (CDFD), Andhra Bank (AB) and State Bank of Hyderabad (SBH)[105] were established in the city.[132] The city is home to the Hyderabad Securities formerly known as Hyderabad Stock Exchange (HSE),[133] and houses the regional office of Securities and Exchange Board of India(SEBI).[134] The growth of the financial services sector has helped Hyderabad evolve from a traditional manufacturing city to a cosmopolitan industrial service centre.[105] Since the 1990s, the growth of information technology (IT), IT-enabled services (ITES), insurance and financial institutions has expanded the service sector, and these primary economic activities have boosted the ancillary sectors of trade and commerce, transport, storage, communication, real estate and retail.[131]Hyderabad's commercial markets are divided into four sectors: central business districts,[135]sub-central business centres, neighbourhood business centres and local business centres.[136]Many traditional and historical bazaars are located throughout the city, Laad Bazaar being the prominent among all is popular for selling a variety of traditional and cultural antique wares, along with gems and pearls stores.[137][138]13% of the population live below the poverty line.[100] According to a 2012 report submitted by GHMC to the World Bank, Hyderabad has 1,476 slums with a total population of 1.7 million, of whom 66% live in 985 slums in the "core" of the city (the part that formed Hyderabad before the April 2007 expansion) and the remaining 34% live in 491 suburban tenements.[101] About 22% of the slum-dwelling households had migrated from different parts of India in the last decade of the 20th century, and 63% claimed to have lived in the slums for more than 10 years.[57]:55 Overall literacy in the slums is 60–80% and female literacy is 52–73%. A third of the slums have basic service connections, and the remainder depend on general public services provided by the government. There are 405 government schools, 267 government aided schools, 175 private schools and 528 community halls in the slum areas.[102]:70 According to a 2008 survey by the Centre for Good Governance, 87.6% of the slum-dwelling households are nuclear families, 18% are very poor, with an income up to 20000 (US$310) per annum, 73% live below the poverty line (a standard poverty line recognised by the Andhra Pradesh Government is 24000 (US$370) per annum), 27% of the chief wage earners (CWE) are casual labour and 38% of the CWE are illiterate. About 3.72% of the slum children aged 5–14 do not go to school and 3.17% work as child labour, of whom 64% are boys and 36% are girls. The largest employers of child labour are street shops and construction sites. Among the working children, 35% are engaged in hazardous jobs.[57A diphtheria immunisation scheme in London, 1941In 1888, Emile Roux and Alexandre Yersin showed that a substance produced by C. diphtheriaecaused symptoms of diphtheria in animals.[21]In 1890, Shibasaburo Kitasato and Emil von Behring immunized guinea pigs with heat-treated diphtheria toxin. Von Behring won the first Nobel Prize in medicine in 1901 for his work on diphtheria. Over the Christmas holiday in 1891 in Berlin, the first attempt to cure a person of diphtheria was made. It succeeded. ... it was the first cure." [22]In 1895, Mulford Company of Philadelphia started production and testing of diphtheria antitoxin in the United States.[23] Park and Biggs described the method for producing serum from horses for use in diphtheria treatment.In 1897, Paul Ehrlich developed a standardized unit of measure for diphtheria antitoxin. This was first ever standardization of biological product and played an important factor in future developmental work on sera and vaccines.In 1901, thirteen St. Louis children died from contaminated diphtheria antitoxin. The horse from which the antitoxin was derived died of tetanus. This incident coupled with a tetanus outbreak in Camden, New Jersey[24] played an important part in initiating federal regulation of biologic products.[25]In 1905, Franklin Royer, from Philadelphia’s Municipal Hospital, published a paper urging timely treatment for diphtheria and adequate doses of antitoxin.[26] In the same year, Clemens Pirquetand Bela Schick described serum sickness in children receiving large quantities of horse-derived antitoxin.Between 1910 and 1911 Béla Schick developed the Schick test to detect preexistent immunity to diphtheria in an exposed person. Only those who were not exposed to diphtheria were preferably vaccinated. A massive five-year campaign was coordinated by Dr. Schick. As a part of the campaign, 85 million pieces of literature were distributed by the Metropolitan Life Insurance Company with an appeal to parents to "Save your child from diphtheria." A vaccine was developed in the next decade, and deaths began declining in earnest in 1924.[27]A poster from the United Kingdom advertising diphtheria immunisation (published prior to 1962).In 1919, in Dallas, Texas, U.S.A., 10 children were killed and 60 others made seriously ill by toxic antitoxin which had passed the tests of the New York State Health Department. Mulford Company of Philadelphia (manufacturers) paid damages in every case.[28]In the 1920s, there were an estimated 100,000 to 200,000 cases of diphtheria per year in the United States, causing 13,000 to 15,000 deaths per year.[6] Children represented a large majority of these cases and fatalities. One of the most famous outbreaks of diphtheria was in Nome, Alaska; the "Great Race of Mercy" to deliver diphtheria antitoxin is now celebrated by the Iditarod Trail Sled Dog Race.In 1926, Alexander Thomas Glenny increased the effectiveness of diphtheria toxoid by treating it with aluminum salts.[29]In 1943, diphtheria outbreaks accompanied war and disruption in Europe. There were 1 million cases in Europe, with 50,000 deaths.In 1948, 68 of 606 children died after diphtheria immunization due to improper manufacture of aluminum phosphate toxoid.In 1974, WHO included DPT vaccine in their Expanded Programme on Immunization fordeveloping countries.In 1975, an outbreak of cutaneous diphtheria in Seattle, Washington was reported .[30]In 1994, the Russian Federation saw 39,703 diphtheria cases. In contrast, in 1990, there had been only 1,211 cases.In early May 2010, a case of diphtheria was diagnosed in Port-au-Prince, Haiti after the devastating 2010 Haiti earthquake. The 15-year-old male patient died while workers searched for antitoxin.[31]In 2013, 3 children died of diphtheria in Hyderabad, India.[32]The disease may remain manageable, but in more severe cases, lymph nodes in the neck may swell, and breathing and swallowing will be more difficult. People in this stage should seek immediate medical attention, as obstruction in the throat may require intubation or atracheotomy. Abnormal cardiac rhythms can occur early in the course of the illness or weeks later, and can lead to heart failure. Diphtheria can also cause paralysis in the eye, neck, throat, or respiratory muscles. Patients with severe cases will be put in a hospital intensive care unit and be given a diphtheria antitoxin. Since antitoxin does not neutralize toxin that is already bound to tissues, delaying its administration is associated with an increase in mortality risk. Therefore, the decision to administer diphtheria antitoxin is based on clinical diagnosis, and should not await laboratory confirmation.[6]Antibiotics have not been demonstrated to affect healing of local infection in diphtheria patients treated with antitoxin. Antibiotics are used in patients or carriers to eradicate C. diphtheriae and prevent its transmission to others. The CDC recommends[12] either:MetronidazoleErythromycin (orally or by injection) for 14 days (40 mg/kg per day with a maximum of 2 g/d), orProcaine penicillin G given intramuscularly for 14 days (300,000 U/d for patients weighing <10 kg and 600,000 U/d for those weighing >10 kg). Patients with allergies to penicillin G or erythromycin can use rifampin or clindamycin.In cases that progress beyond a throat infection, diphtheria toxin spreads through the blood and can lead to potentially life-threatening complications that affect other organs, such as the heart and kidneys. The toxin can cause damage to the heart that affects its ability to pump blood or the kidneys' ability to clear wastes. It can also cause nerve damage, eventually leading to paralysis. About 40% to 50% of those left untreated can die.Diphtheria is fatal in between 5% and 10% of cases. In children under five years and adults over 40 years, the fatality rate may be as much as 20%.[6] As of 2010 it caused about 2,900 deaths down from 6,300 in 1990.[13]Outbreaks, though very rare, still occur worldwide, including in developed nations, such asGermany and Canada. After the breakup of the former Soviet Union in the late 1980s, vaccination rates in its constituent countries fell so low that there was an explosion of diphtheria cases. In 1991, there were 2,000 cases of diphtheria in the USSR. By 1998, according to Red Crossestimates, there were as many as 200,000 cases in the Commonwealth of Independent States, with 5,000 deaths.[14] This was so great an increase that diphtheria was cited in the Guinness Book of World Records as "most resurgent disease".[citation needed]In 1613, Spain experienced an epidemic of diphtheria. The year is known as "El Año de los Garotillos" (The Year of Strangulations) in history of Spain.[15]In 1613, Spain experienced an epidemic of diphtheria. The year is known as "El Año de los Garotillos" (The Year of Strangulations) in history of Spain.[15]In 1659, Cotton Mather described diphtheria as Malady of Bladders in the Windpipe.[16]In 1735, a diphtheria epidemic swept through New England.[17]Before 1826, diphtheria was known by different names across the world. In England, it was known as Boulogne sour throat, as it spread from France. In 1826, Pierre Bretonneau gave the name to disease as diphtérite (from Greek diphthera "leather") describing the appearance of pseudomembrane in the throat.[18]In 1856, Victor Fourgeaud described an epidemic of diphtheria in California.[19]In 1878, Queen Victoria's daughter Princess Alice and her family became infected with it, causing two deaths, Princess Marie of Hesse and by Rhine and Princess Alice herself.In 1883, Edwin Klebs identified the bacterium and named it Klebs-Loeffler bacterium. The club shape of bacterium helped Edwin to differentiate it from other bacteria. Over the period of time, it was called Microsporon diphtheriticum, Bacillus diphtheriae and Mycobacterium diphtheriae. Current nomenclature is Corynebacterium diphtheriae.Friedrich Loeffler was the first one to cultivate Corynebacterium diphtheriae in 1884. He usedKoch's postulates to prove association between Corynebacterium diphtheriae and Diphtheria. He also showed that the bacillus produces an exotoxin.Diphtheria causes a characteristic swollen neck, sometimes referred to as “bull neck”An adherent, dense, grey pseudomembrane covering the tonsils is classically seen in diphtheriaA diphtheria skin lesion on the legThe symptoms of diphtheria usually begin two to seven days after infection. Symptoms of diphtheria include fever of 38°C (100.4°F) or above, chills, fatigue, bluish skin coloration, sore throat, hoarseness, cough, headache, difficulty swallowing, painful swallowing, difficulty breathing, rapid breathing, foul-smelling bloodstained nasal discharge andlymphadenopathy.[8][9] Symptoms can also include cardiac arrhythmias, myocarditis, and cranial and peripheral nerve palsies.
Prevention
Main article: Smallpox vaccine
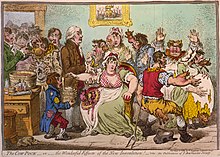
The earliest procedure used to prevent smallpox was inoculation (also known as variolation). Inoculation was possibly practiced in India as early as 1000 BC,[33] and involved either nasal insufflation of powdered smallpox scabs, or scratching material from a smallpox lesion into the skin. However, the idea that inoculation originated in India has been challenged as few of the ancientSanskrit medical texts described the process of inoculation.[34] Accounts of inoculation against smallpox in China can be found as early as the late 10th century, and the procedure was widely practiced by the 16th century, during the Ming Dynasty.[35] If successful, inoculation produced lasting immunity to smallpox. However, because the person was infected with variola virus, a severe infection could result, and the person could transmit smallpox to others. Variolation had a 0.5–2% mortality rate, considerably less than the 20–30% mortality rate of the disease itself.[20]
Lady Mary Wortley Montagu observed smallpox inoculation during her stay in the Ottoman Empire, writing detailed accounts of the practice in her letters, and enthusiastically promoted the procedure in England upon her return in 1718.[36]In 1721, Cotton Mather and colleagues provoked controversy in Boston by inoculating hundreds. In 1796, Edward Jenner, a doctor in Berkeley, Gloucestershire, rural England, discovered that immunity to smallpox could be produced by inoculating a person with material from a cowpox lesion. Cowpox is a poxvirus in the same family as variola. Jenner called the material used for inoculation vaccine, from the root word vacca, which is Latin for cow. The procedure was much safer than variolation, and did not involve a risk of smallpox transmission. Vaccination to prevent smallpox was soon practiced all over the world. During the 19th century, the cowpox virus used for smallpox vaccination was replaced by vaccinia virus. Vaccinia is in the same family as cowpox and variola but is genetically distinct from both. The origin of vaccinia virus and how it came to be in the vaccine are not known.[20]
The current formulation of smallpox vaccine is a live virus preparation of infectious vaccinia virus. The vaccine is given using a bifurcated (two-pronged) needle that is dipped into the vaccine solution. The needle is used to prick the skin (usually the upper arm) a number of times in a few seconds. If successful, a red and itchy bump develops at the vaccine site in three or four days. In the first week, the bump becomes a large blister (called a "Jennerian vesicle") which fills with pus, and begins to drain. During the second week, the blister begins to dry up and a scab forms. The scab falls off in the third week, leaving a small scar.[37]
The antibodies induced by vaccinia vaccine are cross-protective for other orthopoxviruses, such as monkeypox, cowpox, and variola (smallpox) viruses. Neutralizing antibodies are detectable 10 days after first-time vaccination, and seven days after revaccination. Historically, the vaccine has been effective in preventing smallpox infection in 95% of those vaccinated.[38] Smallpox vaccination provides a high level of immunity for three to five years and decreasing immunity thereafter. If a person is vaccinated again later, immunity lasts even longer. Studies of smallpox cases in Europe in the 1950s and 1960s demonstrated that the fatality rate among persons vaccinated less than 10 years before exposure was 1.3%; it was 7% among those vaccinated 11 to 20 years prior, and 11% among those vaccinated 20 or more years prior to infection. By contrast, 52% of unvaccinated persons died.[39]
There are side effects and risks associated with the smallpox vaccine. In the past, about 1 out of 1,000 people vaccinated for the first time experienced serious, but non-life-threatening, reactions including toxic or allergic reaction at the site of the vaccination (erythema multiforme), spread of the vaccinia virus to other parts of the body, and to other individuals. Potentially life-threatening reactions occurred in 14 to 500 people out of every 1 million people vaccinated for the first time. Based on past experience, it is estimated that 1 or 2 people in 1 million (0.000198%) who receive the vaccine may die as a result, most often the result of postvaccinial encephalitis or severe necrosis in the area of vaccination (called progressive vaccinia).[38]
Given these risks, as smallpox became effectively eradicated and the number of naturally occurring cases fell below the number of vaccine-induced illnesses and deaths, routine childhood vaccination was discontinued in the United States in 1972, and was abandoned in most European countries in the early 1970s.[5][40] Routine vaccination of health care workers was discontinued in the U.S. in 1976, and among military recruits in 1990 (although military personnel deploying to the Middle East and Korea still receive the vaccination.[41]) By 1986, routine vaccination had ceased in all countries.[5] It is now primarily recommended for laboratory workers at risk for occupational exposure.[20]
Treatment
Smallpox vaccination within three days of exposure will prevent or significantly lessen the severity of smallpox symptoms in the vast majority of people. Vaccination four to seven days after exposure can offer some protection from disease or may modify the severity of disease.[38] Other than vaccination, treatment of smallpox is primarily supportive, such as wound care and infection control, fluid therapy, and possible ventilator assistance. Flat and hemorrhagic types of smallpox are treated with the same therapies used to treat shock, such as fluid resuscitation. People with semi-confluent and confluent types of smallpox may have therapeutic issues similar to patients with extensive skin burns.[42]
No drug is currently approved for the treatment of smallpox. However, antiviral treatments have improved since the last large smallpox epidemics, and studies suggest that the antiviral drug cidofovir might be useful as a therapeutic agent. The drug must be administered intravenously, however, and may cause serious kidney toxicity.[43]
Prognosis
The overall case-fatality rate for ordinary-type smallpox is about 30%, but varies by pock distribution: ordinary type-confluent is fatal about 50–75% of the time, ordinary-type semi-confluent about 25–50% of the time, in cases where the rash is discrete the case-fatality rate is less than 10%. The overall fatality rate for children younger than 1 year of age is 40–50%. Hemorrhagic and flat types have the highest fatality rates. The fatality rate for flat-type is 90% or greater and nearly 100% is observed in cases of hemorrhagic smallpox. The case-fatality rate for variola minor is 1% or less.[23] There is no evidence of chronic or recurrent infection with variola virus.[23]
In fatal cases of ordinary smallpox, death usually occurs between the tenth and sixteenth days of the illness. The cause of death from smallpox is not clear, but the infection is now known to involve multiple organs. Circulating immune complexes, overwhelming viremia, or an uncontrolled immune response may be contributing factors.[20] In early hemorrhagic smallpox, death occurs suddenly about six days after the fever develops. Cause of death in hemorrhagic cases involved heart failure, sometimes accompanied by pulmonary edema. In late hemorrhagic cases, high and sustained viremia, severe platelet loss and poor immune response were often cited as causes of death.[24] In flat smallpox modes of death are similar to those in burns, with loss of fluid, protein and electrolytes beyond the capacity of the body to replace or acquire, and fulminatingsepsis.[42]
Complications
Complications of smallpox arise most commonly in the respiratory system and range from simple bronchitis to fatalpneumonia. Respiratory complications tend to develop on about the eighth day of the illness and can be either viral or bacterial in origin. Secondary bacterial infection of the skin is a relatively uncommon complication of smallpox. When this occurs, the fever usually remains elevated.[20]
Other complications include encephalitis (1 in 500 patients), which is more common in adults and may cause temporary disability; permanent pitted scars, most notably on the face; and complications involving the eyes (2% of all cases). Pustules can form on the eyelid, conjunctiva, and cornea, leading to complications such as conjunctivitis, keratitis, corneal ulcer, iritis, iridocyclitis, and optic atrophy. Blindness results in approximately 35% to 40% of eyes affected with keratitis and corneal ulcer. Hemorrhagic smallpox can cause subconjunctival and retinal hemorrhages. In 2% to 5% of young children with smallpox, virions reach the joints and bone, causing osteomyelitis variolosa. Lesions are symmetrical, most common in the elbows, tibia, and fibula, and characteristically cause separation of an epiphysis and marked periostealreactions. Swollen joints limit movement, and arthritis may lead to limb deformities, ankylosis, malformed bones, flail joints, and stubby fingers.[7]
History
Main article: History of smallpox
Viral evolution
The date of the appearance of smallpox is not settled. It most likely evolved from a rodent virus between 68,000 and 16,000 years ago.[44][45] The wide range of dates is due to the different records used to calibrate the molecular clock. Oneclade was the variola major strains (the more clinically severe form of smallpox) which spread from Asia between 400 and 1,600 years ago. A second clade included both alastrim minor (a phenotypically mild smallpox) described from the American continents and isolates from West Africa which diverged from an ancestral strain between 1,400 and 6,300 years before present. This clade further diverged into two subclades at least 800 years ago.
A second estimate has placed the separation of variola from Taterapox at 3000–4000 years ago.[46] This is consistent with archaeological and historical evidence regarding the appearance of smallpox as a human disease which suggests a relatively recent origin. However if the mutation rate is assumed to be similar to that of the herpesviruses the divergence date between variola from Taterapox has been estimated to be 50,000 years ago.[46] While this is consistent with the other published estimates it suggests that the archaeological and historical evidence is very incomplete. Better estimates of mutation rates in these viruses are needed.
Other history
The earliest credible clinical evidence of smallpox is found in the Egyptian mummy of Ramses V who died more than 3000 years ago (1145 BC).[9] Historical records from Asia describe evidence of smallpox-like disease in medical writings from ancient India (as early as 1500 BC)[48] and China (1122 BC).[49] It has been speculated that Egyptian traders brought smallpox to India during the 1st millennium BC, where it remained as an endemic human disease for at least 2000 years. Smallpox was probably introduced into China during the 1st century AD from the southwest, and in the 6th century was carried from China to Japan.[24] In Japan, the epidemic of 735–737 is believed to have killed as much as one-third of the population.[10][50] At least seven religious deities have been specifically dedicated to smallpox, such as the god Sopona in the Yoruba religion. In India, the Hindu goddess of smallpox, Sitala Mata, was worshiped in temples throughout the country.[51]
The timing of the arrival of smallpox in Europe and south-western Asia is less clear. Smallpox is not clearly described in either the Old or New Testaments of the Bible or in the literature of the Greeks or Romans. While some have identified the Plague of Athens – which was said to have originated in "Ethiopia" and Egypt – or the plague that lifted Carthage's 396 BC siege of Syracuse with smallpox,[2] many scholars agree it is very unlikely such a serious disease as variola major would have escaped being described by Hippocrates if it had existed in the Mediterranean region during his lifetime.[52] While the Antonine Plague that swept through the Roman Empire in AD 165–180 may have been caused by smallpox,[53] Saint Nicasius of Rheims became the patron saint of smallpox victims for having supposedly survived a bout in 450,[2] and Saint Gregory of Tours recorded a similar outbreak in France and Italy in 580, the first use of the term variola;[2] other historians speculate that Arab armies first carried smallpox from Africa into Southwestern Europe during the 7th and 8th centuries.[24] In the 9th century the Persian physician, Rhazes, provided one of the most definitive descriptions of smallpox and was the first to differentiate smallpox from measles andchickenpox in his Kitab fi al-jadari wa-al-hasbah (The Book of Smallpox and Measles).[54] During the Middle Ages, smallpox made periodic incursions into Europe but did not become established there until the population increased and population movement became more active during the era of the Crusades. By the 16th century smallpox had become well established across most of Europe.[24] With its introduction into populated areas in India, China and Europe, smallpox affected mainly children, with periodic epidemics that killed as many as 30% of those infected. The settled existence of smallpox in Europe was of particular historical importance, since successive waves of exploration and colonization by Europeans tended to spread the disease to other parts of the world. By the 16th century it had become an important cause of morbidity and mortality throughout much of the world. [24]
There are no credible descriptions of smallpox-like disease in the Americasbefore the westward exploration by Europeans in the 15th century AD.[45]Smallpox was introduced into the Caribbean island of Hispaniola in 1509, and into the mainland in 1520, when Spanish settlers from Hispaniola arrived in Mexico bringing smallpox with them. Smallpox devastated the native Amerindianpopulation and was an important factor in the conquest of the Aztecs and theIncas by the Spaniards.[24] Settlement of the east coast of North America in 1633 in Plymouth, Massachusetts was also accompanied by devastating outbreaks of smallpox among Native American populations,[55] and subsequently among the native-born colonists.[56] Some estimates indicate case fatality rates of 80–90% in Native American populations during smallpox epidemics.[57] Smallpox was introduced into Australia in 1789 and again in 1829.[24] Although the disease was never endemic on the continent,[24] it was the principal cause of death in Aboriginal populations between 1780 and 1870.[58]
By the mid-18th century smallpox was a major endemic disease everywhere in the world except in Australia and in several small islands. In Europe smallpox was a leading cause of death in the 18th century, killing an estimated 400,000 Europeans each year.[59]Through the century smallpox resulted in the deaths of perhaps 10% of all the infants ofSweden every year,[10] and the death rate of infants in Russia may have been even higher.[49] The widespread use of variolation in a few countries, notably Great Britain, its North American colonies, and China, somewhat reduced the impact of smallpox among the wealthy classes during the latter part of the 18th century, but a real reduction in its incidence did not occur until vaccination became a common practice toward the end of the 19th century. Improved vaccines and the practice of re-vaccination led to a substantial reduction in cases in Europe and North America, but smallpox remained almost unchecked everywhere else in the world. In the United States and South Africa a much milder form of smallpox, variola minor, was recognized just before the close of the 19th century. By the mid-20th century variola minor occurred along with variola major, in varying proportions, in many parts of Africa. Patients with variola minor experience only a mild systemic illness, are often ambulant throughout the course of the disease, and are therefore able to more easily spread disease. Infection with v. minor induces immunity against the more deadly variola major form. Thus as v. minor spread all over the USA, into Canada, the South American countries and Great Britain it became the dominant form of smallpox, further reducing mortality rates.[24]